Computer-assisted Knee Replacement
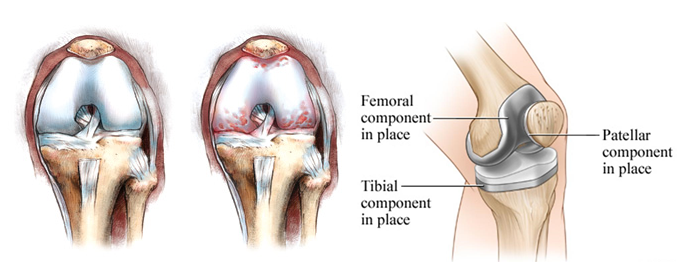
In order to understand what a total knee replacement is, you must first understand the structure of the knee joint. The knee joint is formed by the junction of three bones: the femur (thigh bone), the tibia (shin bone) and the patella (kneecap). These bones are connected to each other by strong ligaments. The powerful muscles of the thigh and calf attach to the bones around the knee by means of tendons. In the healthy knee, these structures work in perfect harmony to move the joint. When your knee is severely arthritic, a total knee replacement will resurface the worn and damaged ends of the femur, tibia and patella with metallic and plastic implants which are fixed to the bone, generally by acrylic cement. This means that the majority of the bone in your knee will be preserved. Only the arthritic cartilage and a thin layer of bone will be removed during the operation.
- The Healthy Knee:
Smooth, slippery, white cartilage covers the contacting surfaces of the knee joint, permitting it to bend and straighten without pain. - The Arthritic Knee:
Over time, the cartilage wears away, leaving the surfaces of the joint pitted, eroded and uneven. The result is stiff, unstable movement and pain. - Total Knee Replacement:
To gain smooth, pain free movement, the end of the femur is resurfaced with a metal implant and the tibia and patella are resurfaced with plastic implants or implants made of both metal and plastic.
This operation has proven to be highly successful in millions of patients worldwide. At Hospital for Special Surgery, we have performed over 60,000 total knee replacements. The operation has been perfected over time with the introduction of improved knee replacement designs and the development of instrumentation that allow precision implantation through limited incisions.
Pre-admission testing that includes blood work, electrocardiogram, chest x-rays, among others; is performed within 30 days of surgery. The same day, patients will be seen by one of our internists to be cleared medically before the surgery. An educational class and book will be given reviewing all the aspects of admission, hospitalization and recovery. The hospital’s social worker will discuss the discharge plan to your home or to a rehabilitation center.
Patients are admitted on the day of surgery. Most of the knee replacement operations take from one to one and a half hours depending on the complexity of the deformity of your knee. Most patients prefer to sleep during the operation. In the vast majority of patients an epidural anesthesia is performed, leaving the epidural catheter in for 24 hours, through which the patient can self-administer analgesics via a pump for pain control. In addition, a nerve block may be administered by your anesthesiologist. I will also give anesthetic medication in your incision. With these gestures, the postoperative pain is minimal. After the epidural catheter is removed, analgesics are given by mouth, intravenously or intramuscularly.
The incision is made in the front of the knee. It is approximately 4 to 6 inches long, depending on weight, musculature, and the complexity of the knee deformity. During surgery, a computer device is used to make sure the knee replacement parts are properly positioned and that the ligaments that will “guide” the motion of the knee replacement parts after surgery are adequately balanced. These two factors are necessary for your knee replacement to function well, minimize wear, and improve range of motion and function.
After the operation, patients remain in the Recovery Room where they are closely monitored and supervised. Patients are moved to their rooms after several hours or the next morning after being cleared by the internist or anesthesiologist. Patients usually sit and stand on the day of surgery or the next day, and walk with the aid of a walker, progressing to a cane in the next few days. You will be instructed to do exercises to increase progressively your range of motion and gain muscle strength before and after your discharge from the hospital. You will need to be fully involved with the physical rehabilitation of your knee to achieve the best possible result.
Patients are discharged home when they can ambulate well with the use of a cane and can do stairs independently, holding the banister, around the second or third day after surgery. At the time of discharge, written instructions are given, outlining the Do’s and Don’ts and exercises.
Patients who live alone, who progress slowly, or with other limitations, can be discharged to a rehabilitation center, if the medical insurance covers it. Please discuss the discharge plan with my staff and the hospital’s social worker.
Patients are seen by me five to six weeks after surgery for a clinical and radiographic examination, and according to their progress, new exercises and written instructions are given. Patients should be able to walk without the use of a walking aid in about four to six weeks, and the maximum benefit is usually achieved a few months after surgery.
In our experience, total knee replacement has been highly successful in relieving pain, improving ambulation and knee motion, and reducing disability. None of the results previously mentioned, however, can be guaranteed, as there is a certain risk of complications. The complications are rare, and include infection, stiffness of your knee after surgery, nerve/vascular damage, clot formation, and other medical problems. In each case, patients are carefully analyzed and treated accordingly so as to avoid complications, trying to achieve the best possible result.
This is a brief description and should serve as a general guideline only since each patient is different and the potential for recuperation and complications varies widely according to age, general health, type of knee problem, previous operations, etc. Copies of the instructions given at the time of discharge, at six weeks after surgery, the precautions the patient should follow to protect the artificial knee, and information about orthopedic devices and risks of complications are available upon request.
I encourage you to discuss any questions that you may have regarding the operation or any other medical aspects with me. Other questions regarding insurance coverage, dates, scheduling, etc. should be directed to my staff.
For additional information, instructions and educational videos please visit VIDEO LIBRARY




