Partial Knee Replacement
In order to understand what a partial knee replacement is, you must first understand the structure of the knee joint. The knee joint is formed by the junction of three bones: the femur (thigh bone), the tibia (shin bone) and the patella (kneecap). These bones are connected to each other by strong ligaments. The powerful muscles of the thigh and calf attach to the bones around the knee by means of tendons. In the healthy knee, these structures work in perfect harmony to move the joint. There are three major compartments in your knee (see image below): The Medial compartment (located on the inner side), the Lateral compartment (located on the outer side), and Anterior (located in the front of the knee between the kneecap and the thigh bone). When two or more compartments of your knee are severely arthritic or damaged, a total knee replacement will completely resurface the ends of the femur, tibia and patella with metallic and plastic implants which are fixed to the bone, generally by acrylic cement. A selected group of patients will present with isolated arthritis on one of the three compartments (generally the inner one) and may benefit from a partial knee replacement, in which only the arthritic, damaged compartment is resurfaced.
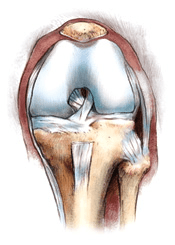
The healthy knee: Smooth, slippery, white cartilage covers the contacting surfaces of the knee joint, permitting it to bend and straighten without pain.
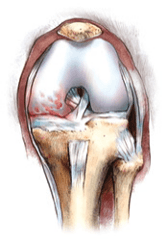
The unicompartimental arthritic knee: The cartilage wears away in one of the three compartments, leaving the surfaces of the joint pitted, eroded and uneven. The result is unstable movement and pain.
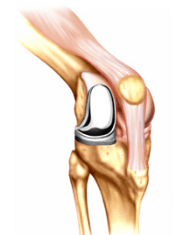
Partial Knee Replacement: To gain smooth, pain free movement, the end of the femur and the tibia in the affected compartment are resurfaced with a metal and plastic implant. The healthy compartments and all the ligaments of the knee remain intact.
Since only one compartment is replaced, the operation can be performed through a relatively smaller incision, with less soft tissue dissection and blood loss than the ones required for a total knee replacement. For all these reasons, the patients generally experience a faster recovery, and less pain than those experienced following a total knee replacement.
Your surgeon may request additional studies prior to recommending a partial knee replacement. An MRI may provide information on the condition of the cartilage in the knee.
In the properly selected patient, partial knee replacement is a durable operation that provides pain relief, and improves ambulation and function. The operation has been perfected over time with the introduction of new prosthetic designs and the development of instrumentation that allow precise implantation through limited incisions.
Partial knee replacements have a risk of mechanical failure (loosening and plastic wear). With partial knee replacement, there is a risk for degenerative arthritis developing in other compartments of the knee. Most of the revisions of failed partial knee replacements can be done using implants regularly used for total knee replacements.
Pre-admission testing that includes blood work, electrocardiogram, chest x-rays, among others; is performed 10 days prior to surgery. The same day, patients will be seen by one of our internists to be cleared medically before the surgery. An educational class and book will be given reviewing all the aspects of admission, hospitalization and recovery. A social worker will discuss the discharge plan to your home or to a rehabilitation center.
Patients are admitted on the day of surgery. Most of the knee replacement operations take from one to one and a half hours. Most patients prefer to sleep during the operation. In the vast majority of patients an epidural anesthesia is performed. In addition, a nerve block may be administered by your anesthesiologist. With this method, the postoperative pain is minimal. After the epidural catheter is removed, analgesics are given by mouth, intravenously or intramuscularly.
The incision is made in the front of the knee. It is approximately 3 to 5 inches long, depending on weight, musculature, and the complexity of the knee deformity. After the operation, patients remain in the Recovery Room where they are closely monitored and supervised. Patients remain at bed rest overnight, and according to pain, wound healing and other factors, they usually sit and stand on the next day after surgery, and walk with the aid of a walker, progressing to a cane in the next few days. Selected patients can be discharged home on the same day. You will be instructed to do exercises to increase progressively your range of motion and gain muscle strength before and after your discharge from the hospital. You will need to be fully involved with the physical rehabilitation of your knee to achieve the best possible result.
Most patients are discharged home when they can ambulate well with the use of a cane and can do stairs independently, holding the banister, around the third day after surgery. At the time of discharge, written instructions are given, outlining the Do’s and Don’ts and exercises. Those patients who live alone, who progress slowly, or with other limitations, can be discharged to a rehabilitation center, if the medical insurance covers it. Please discuss the discharge plan with my secretary and the social worker.
Thereafter, patients are seen by me about six weeks after surgery for a clinical and radiographic examination, and according to their progress, new exercises and written instructions are given. Patients should be able to walk without the use of a walking aid in about three to four weeks, and the maximum benefit is usually achieved a few months after surgery.
In our experience, partial knee replacement has been highly successful in relieving pain, improving ambulation, function, and reducing disability. None of the results previously mentioned, however, can be guaranteed, as there is a certain risk of complications. The complications are rare, and include infection, stiffness of your knee after surgery, nerve/vascular damage, clot formation, and other medical problems. In each case, patients are carefully analyzed and treated accordingly so as to avoid complications, trying to achieve the best possible result.
This is a brief description and should serve as a general guideline only since each patient is different and the potential for recuperation and complications varies widely according to age, general health, type of knee problem, previous operations, etc.
Copies of the instructions given at the time of discharge, at six weeks after surgery, the precautions the patient should follow to protect the artificial knee, and information about orthopedic devices and risks of complications are available upon request.
Thank you for reading this information carefully. Please be encouraged to discuss any questions that you may have regarding the operation or any other medical aspects with me. Other questions regarding insurance coverage, dates, scheduling, etc. should be directed to my secretary.
Additional information, instructions and educational videos can be obtained at www.agdvmd.com




